Differentiating contrast extravasation vs. haemorrhagic transformation after mechanical thrombectomy
By Antonio Ciacciarelli1 & Barbara Casolla2
1Department of Clinical and Experimental Medicine, University of Messina, Italy
2 Unité Neuro-vasculaire, CHU Nice, Université Cote D’Azur, Nice, France
Twitter: @a_ciacciarelli; @BarbaraCasolla
Since the time window for acute reperfusion treatments in ischemic strokes has been extended, the number of patients treated by mechanical thrombectomy (MT) increased. Accordingly, we observe more and more frequently cerebral hyperdensities on post-procedural Computed Tomography (CT): however, in routine clinical practice, distinguishing between iodine contrast media extravasation and haemorrhagic transformation may be challenging.
The incidence of post-procedural cerebral hyperdensities (PCH) varies according to delays between revascularization and CT performance, ranging from 60% when brain CT is performed within 4,5 hours after MT 1, to 30% at 24 hours. When PCH disappear after repeated CT scan, they likely represent contrast extravasation, because contrast is washed out, whereas haemorrhagic transformation persists on follow-up neuroimaging 2.
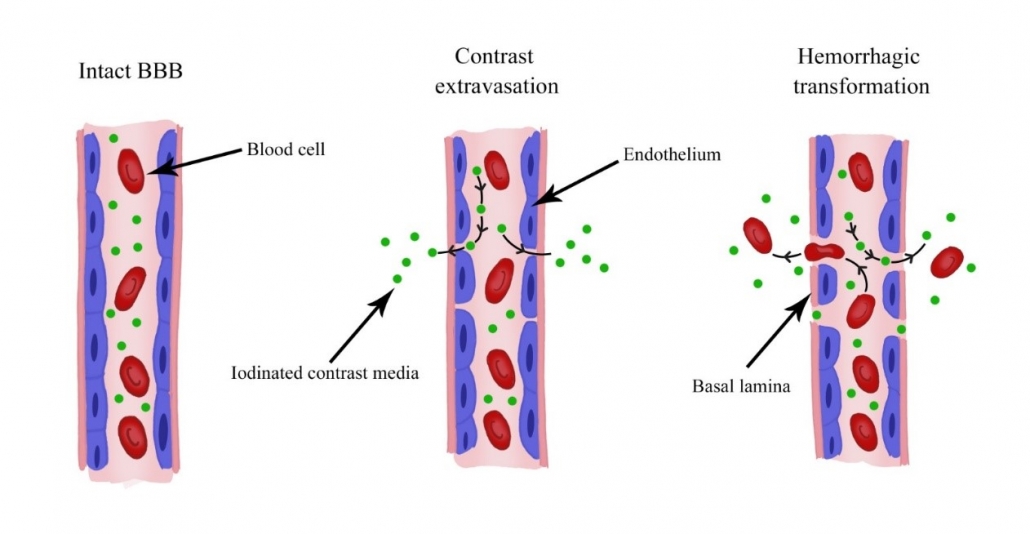
From a physiopathological point of view, either blood or contrast extravasation presuppose blood-brain barrier (BBB) disruption. However, cellular blood elements need a BBB rupture extending to basal lamina to leak into the brain tissue 3 (figure).
Some authors investigated neuroimaging methods that could help distinguishing contrast extravasation from haemorrhagic transformation on CT. Indeed, hounsfield unit (HU) on conventional non enhanced CT can help when PCH attenuation is less than 50 HU on immediate post procedure CT scan, which allows excluding a haemorrhagic transformation, however, the sensitivity is low (56%)2. Dual-Energy CT (DECT) image acquisition is acquired by using two different x-ray energy levels, and it is considered the gold standard to distinguish between blood and contrast, with an overall sensitivity of 100% and specificity of 93% 4. Gradient Echo (GRE) on Magnetic Resonance Imaging (MRI) allows differential diagnosis: haemorrhagic transformation shows an hypointense signal, while contrast extravasation appears iso- or hyper-intense 5.
The clinical impact of PCH is uncertain and whether contrast extravasation itself independently predicts poor outcome after endovascular therapy is unknown 6. Indeed, contrast extravasation is also associated with an increased risk of haemorrhagic transformation, suggesting an underlying vessel injury. Consistently, BBB leakage before reperfusion therapy is independently associated with an increased risk of symptomatic haemorrhagic transformation 7.
From a therapeutic point of view, the presence of a haemorrhagic transformation often delays the introduction of antithrombotic drugs and an early differentiation between blood and contrast is crucial for a prompt start of the therapy. However, whether contrast extravasation, by means of a damaged BBB, may be a warning sign for future risk of brain haemorrhage needs to be further investigated.
For future research directions, studying contrast extravasation after MT may help quantitively measuring early BBB disruption, with important clinical implications: individual-level prediction of further haemorrhagic transformation after antithrombotic drug introduction, therapeutic effect of drugs targeting BBB and, potentially, candidate selection for neuroprotective agents.
REFERENCES
- Nikoubashman O, Reich A, Gindullis M, Frohnhofen K, Pjontek R, Brockmann M-A, Schulz JB, Wiesmann M. Clinical significance of post-interventional cerebral hyperdensities after endovascular mechanical thrombectomy in acute ischaemic stroke. Neuroradiology. 2014;56:41–50.
- Payabvash S, Qureshi MH, Khan SM, Khan M, Majidi S, Pawar S, Qureshi AI. Differentiating intraparenchymal hemorrhage from contrast extravasation on post-procedural noncontrast CT scan in acute ischemic stroke patients undergoing endovascular treatment. Neuroradiology. 2014;56:737–744.
- Hamann GF, Okada Y, Del Zoppo GJ. Hemorrhagic transformation and microvascular integrity during focal cerebral ischemia/reperfusion. J. Cereb. Blood Flow Metab.
- Phan CM, Yoo AJ, Hirsch JA, Nogueira RG, Gupta R. Differentiation of hemorrhage from iodinated contrast in different intracranial compartments using dual-energy head CT. Am. J. Neuroradiol. 2012;33:1088–1094.
- You SH, Kim B, Kim BK, Suh SI. MR imaging for differentiating contrast staining from hemorrhagic transformation after endovascular thrombectomy in acute ischemic stroke: Phantom and patient study. Am. J. Neuroradiol. 2018;39:2313–2319.
- Renú A, Amaro S, Laredo C, Román LS, Llull L, Lopez A, Urra X, Blasco J, Oleaga L, Chamorro Á. Relevance of Blood–Brain Barrier Disruption After Endovascular Treatment of Ischemic Stroke. 2015;46:673–679.
- Arba F, Piccardi B, Palumbo V, Biagini S, Galmozzi F, Iovene V, Giannini A, Dario Testa G, Sodero A, Nesi M, et al. Blood‐Brain‐Barrier Leakage and Hemorrhagic Transformation: the Reperfusion Injury in Ischemic StroKe (RISK) study. Eur. J. Neurol. 2021.